Indiana University Center for Bioethics
Ethics Guide for Health Care Practitioners
Working Under Conditions of an Influenza Pandemic
August 2009
In July 2008, a nation-wide Summit of the States convened in Indianapolis, Indiana to address the ethical issues arising for state-level health officials planning for pandemic influenza. www.bioethics.iu.edu/pandemic_portal.asp
One of the action steps identified at the Indianapolis Summit was to: “Create toolkits for local education, planning, partnerships, and community engagement.”
You now have in your hands an Ethics Toolkit for Health Care Practitioners that has been developed by the Indiana University Center for Bioethics, with funding from the Centers for Disease Control and Prevention through the Indiana State Department of Health.
The Ethics Toolkit is designed to assist health care providers in carrying out their ethical responsibilities of caring for patients and families within the clinical environment during an influenza pandemic. In particular, the Toolkit is designed to give practical input on key issues facing health care practitioners, specifically: Altered Standards of Care; Vaccine and Antiviral Provision; Triage; and Workforce Management. Other issues are discussed in the Toolkit, but receive less comprehensive attention. The input for each of these issues is based on an Ethical Framework that provides a reasoned basis for decision making. The Framework – Ethical Points to Consider – is found on the following page.
The Toolkit is intended to supplement relevant institutional, state and federal policies and procedures, not to replace them. Health care practitioners are encouraged to discuss policies applicable to their work, with the appropriate institutional official. Practitioners are given resources such as web-links, for further information.
Ethical Points to Consider
Transparency
No policy can be developed, much less implemented, without an assurance that its justification and rationale have been made clear to those who will be affected by it. Maintaining transparency and open communication enhances the public’s trust in the decision-makers and may assist in achieving public compliance to control measures.
Public Accountability
In the event of an influenza pandemic crisis, policymakers are obligated to include a method for ensuring ethical guidelines and procedures are upheld in order to avoid an erosion of trust and transparency with the public. Should an error or oversight occur, it is the responsibility of the policymakers to acknowledge the situation and address the public promptly in order to resolve the resulting complications. Decision-makers should be prepared to accept responsibility if errors or complications occur and be accountable for correcting such flaws.
Responsiveness
While it is often accepted that public health actions should ultimately be determined by experts, involving the public can help build trust and increase acceptance of the proposed policy. Public engagement may occur along a continuum from no engagement to active partnering. Responsiveness involving the willingness to address the concerns of the public and of health care professionals is essential.
Proportionality
Policies and procedures should be based on sound scientific evidence or on the best evidence available. In addition, the policy’s measures should reflect the severity of the situation while remaining as minimally invasive as possible. Proportionality involves weighing the perceived benefits of a policy with the burdens of implementation. No group should bear a disproportionate burden in a pandemic emergency.
Reciprocity
In the event of an influenza pandemic crisis, certain communities and individuals may face increased risk of illness and/or restrictions on their autonomy. If leaders expect people exposed to or suffering from communicable diseases to act in a manner that does not put others at risk, it is important that they create a social environment that does not leave people without supports. These may include access to protective equipment, medication, and other supplies.
Uniformity of Implementation
Consistency in the implementation and application of the policy helps to ensure that similar cases will be treated equally. This will aid in limiting unnecessary discrimination and may assist in conveying the policy’s fairness to the public and to the affected parties. Institutions may determine what, if any, exceptions may be made to the policy.
Index
Altered Standards of Care
Vaccine and Antiviral Allocation
Triage
Patient Guide
Resources
References
Altered Standards of Care
Case studies
Case #1: Three weeks into the first pandemic wave, the intensivist who has been directing care at a hospital has become ill and a replacement is found. The new physician, an internist who had been staffing at an alternate care site, expresses deep anxiety about the rigid triage criteria in use, and he states he will not abide by them because of fear of being sued for malpractice. What can be done?
Case #2: After the pandemic begins, a hospital reports that 30% of its workforce has become ill, and another 25% has refused to report to work. Several people have offered to volunteer at the hospital to supplement its workforce. How can the hospital identify appropriate volunteers?
FAQs
1. What triggers Altered Standards of Care?
This is a local issue that may vary according to the community and state, but the actual trigger and the mechanism for declaring the implementation of ASC should be clearly identified, and the means of publicizing the new state of affairs should be well planned.
2. How will decisions be made, by whom and who is second in command?
The decision-making hierarchy will be established locally and every health care institution should develop a clear medical chain of command, including backup personnel. It is also strongly recommended that hospitals in certain regions – for example a health district or set of counties, or the state, etc. – abide by the same triage and altered standards of care protocols in order to ensure a more fair distribution of scarce resources and to discourage patients from traveling desperately among hospitals seeking extended care.
3. How will Altered Standards of Care be communicated to patients, families and health care professionals?
This is probably the most critical piece of all the preparations. All persons must recognize that if a pandemic develops, health care as we all know it in the US could radically shift from a ‘what is best for this individual patient’ to ‘what is best for this group’ focus. In ethics terminology this ‘greatest good for the greatest number’ approach is called ‘Utilitarianism,’ or ‘Consequentialism.’ It is a well-respected ethical theory, but it is not the dominant ethics driving medicine in the United States except in some matters of Public Health. In the event of a pandemic, it will be imperative, ethically and medically, to align health care with the ethics of doing the best for the larger group, but it will be traumatic and terribly difficult for all concerned.
After a clear and full explanation of the above rationale for the shift in how and what health care will be provided, all facilities must also publish their clear and explicit new guidelines for treatment and the options available for those who will not receive acute treatment. Information should be consistent, transparent, and widely shared within each community and within each state. In addition, all facilities should have the means to respond to emotional and spiritual needs of the public and professionals involved.
4. Who does what?
- See Personnel section
5. Where will care take place? What if hospitals are full?
- See Place of Care section
6. Are there any models for delivering Altered Standards of Care?
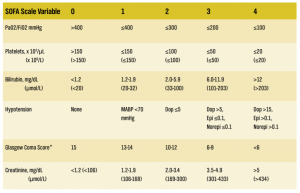
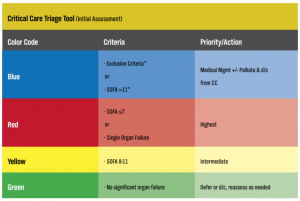
- See the SOFA Scale and Critical Care Triage Tool chart
Altered Standards of Care will affect the actual clinical care able to be provided, the place of care, and the personnel involved in all aspects of health care provision
Place of Care
Pandemic influenza will require planners to consider alternate care sites for health care delivery, quarantine and isolation, and mortuary services if hospitals and morgues become overwhelmed.
A best practice approach is obtained through partnership and agreement with the owners of facilities (e.g., schools, stadiums, etc.) that may be used.
Type of Care
In-home care provided by home-care personnel, family, and friends may need to be encouraged.
Personnel
Institutions should consider how to anticipate and address staffing shortages because the alteration of staff members’ regular responsibilities may result in increased stress for the affected staff or a decreased quality of the usual care.
Health care institutions should ensure a comprehensive program is developed and implemented to provide all health care workers with adequate training and information regarding pandemic influenza and their anticipated responsibilities.
Planning
- Planning for Altered Standards of Care is controversial; however, it is imperative. It is strongly advised that each institution have a triage plan in place for altered standards of care.
- A proposed model for triage using SOFA scores and a proposed model for a method to assess incoming patients appear at the end of this section. It is up to the discretion of the institution to choose whether or not to adopt any of this material or to develop other protocols.
Sequential Organ Failure Assessment (SOFA) Score
SOFA Scale
Dopamine [Dop], epinephrine [Epi], norepinephrine [Norepi] doses in ug/kg/min SI units in brackets
Adapted from: Ferreira Fl, Bota DP, Bross A, Melot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA 2001; 286(14): 1754-1758.
Explanation of Variables:
PaO2/FiO2 indicates the level of oxygen in the patient’s blood.
Platelets are a critical component of blood clotting.
Bilirubin is measured by a blood test and indicates liver function.
Hypotension indicates low blood pressure; scores of 2, 3, and 4 indicate that blood pressure must be maintained by the use of powerful medications that require ICU monitoring, including dopamine, epinephrine, and norepinephrine.
*The Glasgow Coma Score is a standardized measure that indicates neurologic function; low score indicates poorer function. Creatinine is measured by a blood test and indicates kidney function.
Below is one example of how the SOFA scores can be used in a modified version of the OHPIP Triage Tool. The website reference is listed in the Resource section of this Toolkit.
Adapted Ontario Health Plan for an Influenza Pandemic (OHPIP) Triage Tool
*If exclusion criteria or SOFA >11 occurs at any time from the initial assessment to 48 hours, change triage code to Blue and palliate. CC = critical care. d/c = discharge.
Ethical Points to Consider Reflected in Altered Standards of Care
Transparency
Providing the public and health care providers with information regarding alterations in health care procedures will help to achieve compliance with these procedures. Discussions with citizens and faith-based communities regarding potential barriers to adherence to funeral and burial procedures will prepare these communities for potential delays and alterations that may occur while attempting to follow cultural practices. By making these communities aware of these implications prior to the event, they may be more likely to comply with the necessary course of action.
Responsiveness
Through partnerships with owners/administrators of potential alternate care sites, planners may develop procedures that will ensure the public’s health needs are met, while assuring owners their facilities will be properly insured and protected.
Proportionality
Alternate care sites are to be used only when hospitals lack sufficient capacity; alternate staffing procedures are to be used only during a staffing shortage; and documentation procedures are to switch to truncated procedures only when current standards are impossible to maintain given a large patient influx. Patients must sacrifice privacy and confidentiality only when absolutely necessary to maintain a functioning care facility.
Reciprocity
Providing legal protection and mental health services to health care workers will help to ease the disproportionate amount of burden they will bear. Preparing these workers prior to a pandemic will reduce the stress they will face. Providing additional security also will help to ease the burden on health care professionals, since they will be more able to perform their duties in the absence of fear. Furthermore, meeting the basic needs of these workers, such as providing housing for non-local volunteers, will help to reduce stress and retain these staff members.
Case Study Responses
Case #1: Upon the declaration of a pandemic influenza emergency, legal protections may be put into place to protect health care workers who follow altered standards protocols from litigation. These measures will vary accordingly to location. The new physician should be informed of these legal protections and the necessity to follow altered standards protocol to ensure fair and consistent implementation.
Case #2: It may be advisable for hospitals to have a database of potential alternate health care workers whose skills and qualifications have been assessed prior to the occurrence of the pandemic. These may include retired nurses and physicians, as well as medical and nursing students.
Vaccine and Antiviral Allocation
Case Studies
Case #1: A clinic has one remaining bottle of oseltamivir. A married 34-year-old woman presents to the clinic with her 5-year-old son. The woman has been experiencing fever, cough, muscle aches, and sore throat for 24 hours. Her physiological assessment reveals that she is eligible to receive treatment, a 5-day course of oseltamivir. The boy shows no symptoms of infection, and his physiological assessment reveals that he is not eligible to receive the medication. The woman says her husband also is not showing signs of infection. She requests that she not receive the medication so that her treatment can be given to her son for use as prophylaxis. Who should receive the oseltamivir?
Case #2: A vaccine for the pandemic influenza has been developed but is still in extremely limited supply. A 47-yearold pulmonologist qualifies to receive this vaccine. He requests that his family also be vaccinated. His wife is a healthy 44-year-old who works from home. His two children are 16 and 17 with no known immune system impairment. The pulmonologist states that he will not report to work without his family being vaccinated. What should be done?
FAQs
- If an effective vaccine is available, who will qualify to receive it? Who decides?
- See Planning and Implementation sections
- If an effective antiviral medication is available, who should get it? Should the medicine be used for treatment, prophylaxis, or post-exposure prophylaxis?
- See Antiviral Use section
Effective vaccines may not be available at the beginning of a pandemic. When an effective vaccine is available, quantities may be insufficient to treat everyone in a community at the same time. Antiviral medications, if effective, may also be in short supply; thus, every community must develop a plan for fair allocation of both vaccines and medications.
Planning
Vaccine priority groups are established by federal agencies. Federal and state stockpiles of antivirals may only be used for treatment and there is no priority list for their use. If there is an abundance of antivirals then health care facilities should be aware of other prioritization guidelines in their community.
Implementation
Policies must be implemented consistently to ensure fairness and equal opportunity for care.
Antiviral Use
Differences between prioritization lists primarily are the result of differences in views on the purpose of antiviral use, whether for prophylaxis, post-exposure prophylaxis, or treatment.
- Prophylaxis is the provision of antiviral treatment in order to prevent illness in individuals who may not necessarily have been exposed to the virus. It may be used early in the pandemic in order to prevent the spread of the illness throughout an affected community.
- Post-exposure prophylaxis is the provision of the antiviral to individuals who are known to have been in close contact with an infected individual, such as a family member.
- Treatment is the use of antivirals in individuals who have a documented infection or exhibit signs of infection. It is most effective if dispensed in the first 48 hours of symptoms.
Should have an influenza pandemic plan, which addresses vaccine and antiviral administration and storage. n Should ensure that providers understand policies regarding the prioritization and utilization of antivirals and vaccines. n Should emphasize the use of non-pharmaceutical prophylaxis, such as the use of personal protective equipment, hand washing, and good respiratory hygiene.
Points to consider in the proposed prioritization strategy for antivirals and vaccines
Transparency
The inclusion of open communication facilitates public awareness of the prioritization policies and their implications.
Responsiveness
Public and professional input in the decision-making process, along with the presence of communication mechanisms, allows for the iterative evaluation and improvement of the prioritization guidelines.
Reciprocity
Health care workers engaged in direct patient care and emergency response personnel will be at highest risk of infection and are prioritized for protective equipment and vaccines to minimize their increased risk of infection and allow them to fulfill their duties.
Case Study Responses
Case #1: The woman should be informed that the medication is to be used for treatment only and that an assessment of her son’s health revealed that he did not qualify for this. Additionally, prophylaxis generally requires four courses of medication, so the one bottle she would provide him likely would be insufficient. If the woman continues to refuse the medication, it should be saved for the next qualifying patient. If she accepts the medication, the first dose should be given at the clinic so as to ensure she is the one taking the medicine and that she is not providing it to her son. She should be informed of the potential complications involved in giving the child medication that is intended for an adult. Additionally, she should be informed of non-pharmaceutical methods of preventing transmission of the virus to her son and husband, such as frequent hand washing, isolating herself in the household, and allowing her husband to care for their son to the extent possible.
Case #2: Though the pulmonologist qualifies as a top priority for vaccination due to his occupation and direct exposure to patients, his wife and adolescent children likely do not qualify in times of extreme scarcity due to their relatively low prioritization rankings and limited risk factors. The pulmonologist and his family should be educated on non-pharmaceutical ways to protect themselves from exposure and illness, such as proper hand washing and social distancing. The doctor should then be encouraged to report to work given his specialized skill set and the needs of the community.
Triage
Case Studies
Case #1: A 67-year-old housekeeper and a 24-year-old medical student present to the emergency room with pandemic influenza. An unemployed 39-year-old also presents after having been in a motor vehicle accident. All patients require a ventilator to survive, but the hospital has only one available. Who should get the ventilator?
Case #2: After two weeks of implementing triage criteria that were developed for pandemic use, several physicians begin to question the methodology they have been instructed to use. They express their concerns to their supervisor and state that they would like to implement alternative triage methodologies. What steps should be taken?
FAQs
- Does every hospital need a triage protocol?
- Yes, see Planning section
- If a triage protocol is in use during a pandemic, will it also apply to patients who are hurt or sick with non-pandemic illness?
- Yes, see Proportionality section in the Points to Consider chart
- What if 2 people arrive at a hospital with exactly the same triage admission criteria? What method should be used to break the tie?
- See Planning section and Case Study #1 response
- What should health care providers do if they seriously disagree with or question the protocol?
- See Implementation section and the Responsiveness section in the Points to Consider chart
In the event of a pandemic, critical resources will be in short supply, insufficient to meet the needs of the community. Every facility must develop a just, comprehensive and efficient system of triage for critical resources including health care personnel, beds, medications, equipment (such as ventilators) before a pandemic develops, and clear communication of policies related to all the above.
Planning
Every hospital should have a triage protocol, which includes ethically sensitive tie-breaking criterion.
Implementation
It is imperative that acute care providers are aware of the hospital’s triage protocol.
Hospitals in the same region should abide by the same triage protocols. Acute care facilities should adopt a common procedure to conduct a daily retrospective review of all triage decisions in order to provide accountability and identify areas of the protocol in need of improvement.
Points to Consider Reflected in the Proposed Triage Protocol
Public Accountability
Objective decision-making procedures eliminate subjectivity and bias from the triage protocol. As a result, allocation decisions will be able to withstand public scrutiny.
Responsiveness
The inclusion of an appeals process may be considered to allow health care workers and the general public to voice concern and dissent. Evaluation of these appeals may result in more effective and acceptable triage protocol.
Proportionality
Less drastic methods of preserving scarce resources, such as canceling elective surgeries, are recommended prior to the implementation of rationing procedures. As need becomes greater and resources become more scarce, the policy’s inclusion and exclusion criteria become more restrictive, reflecting the severity of the situation.
Reciprocity
The protocol provides various means of support to affected individuals. For example, those individuals denied access to scarce resources (e.g., ventilators) are provided other means of medical attention, such as palliative care, and those with emotional and psychological burdens resulting from the crisis (e.g., health care workers) are provided appropriate mental health support.
Uniformity of Implementation
The analysis of objective physiological data creates less variation in triage decisions than subjective considerations would create.
Case Study Responses
Case #1: Triage criteria must be applied to all acute care patients, including those not presenting with pandemic influenza. The decision of who receives the ventilator should depend solely on the patients’ physiological prognoses, which are calculated in this example using the SOFA prognostic scoring method, which does not include age or social role of the patient in the decision-making process. Health care facilities must have ethically sensitive tie-breaking criteria in the event that two or more patients have an identical prognosis.
Case #2: Review of triage decisions should be made daily at the institutional and state levels, and any areas identified to be in need of improvement during this review must be communicated quickly and efficiently between the state and the institutions. The physicians’ concerns should be evaluated to determine whether a change should be made. The physicians, however, should not depart from the protocol until such a departure is deemed necessary by protocol reviewers.
Workforce Management
Case Studies
Case #1: A 42-year-old single father works as a custodian at a local hospital. He has two children, ages 7 and 9, both of whom have developed respiratory symptoms within the past 24 hours. Due to a shortage of janitorial staff, the man is called into work. He refuses to report to the hospital in order to remain at home with his sick children. He has no family members in the immediate area who would be able to care for his children in his absence. Given that custodians are not subject to professional codes of ethics or obligations, how should the hospital respond to the employee’s refusal to report to work?
Case #2: A hospital has begun stockpiling personal protective equipment for its employees. When the influenza pandemic begins, the hospital only has enough supplies to cover half its workforce. Neighboring health care facilities also have limited supplies and are unable to provide assistance. What steps must the hospital take to address this situation?
FAQs
- Does a health care professional (nurse, physician, respiratory therapist, etc.) have a professional, ethical, or legal duty to work in a pandemic emergency?
- See Duty to Care and Duty to Report sections
- Does a non-professional staff member have a duty to work in a pandemic emergency?
- See Duty to Report section and Proportionality section in the Points to Consider chart
- Can an institution or the state require anyone to work during a pandemic?
- See Proportionality section in the Points to Consider chart
- What obligation does a health care facility have toward its staff?
- See Duty to Report section and the Points to Consider chart
- Should there be rewards for working and penalties for absenteeism?
- See Response to Absenteeism
In the event of a pandemic, it will be necessary to identify health care workers, professional and nonprofessional, who are critically necessary. The scope and place of work and the notions of risk, duty, absenteeism, and liability may be different under ASC conditions and should be discussed and acknowledged. Policies should be developed and clearly communicated.
Points to Consider Reflected in the Proposed Triage Protocol
Duty to Care
Professional and non-professional staff should be aware of ethical obligations and professional duties during the time of an influenza pandemic. Clear expectations should be conveyed to both professional and non-professional staff.
Health care workers and health care professionals are faced with the risk of being infected while providing care to both infected and exposed patients. Most health care professionals are bound by a code of ethics that obligates them to provide care to patients, which gives rise to several ethical concerns:
-
- What degree of risk is acceptable in occupational exposure? n Should the obligation to provide care diminish with rising levels of risk?
- Is there a level of risk at which the duty to care no longer remains?
- How should health care workers balance competing obligations when they come into conflict, such as when obligations to family clash with obligations to patients?
- Is the obligation to treat absolute?
Duty to Report
Health care organizations should identify and designate health care workers, clinical and nonclinical, deemed to be critically necessary during a pandemic. Health care facilities should have adequate supplies of PPE and other related materials and ensure that these supplies are readily available to all critical personnel expected to interact with patients as appropriate to the situation. Hospital administrators should disperse clear policies regarding:
-
- Type of work expected to be performed
- Obligation to work
- Absenteeism
- Professional standards including: Liability, Negligence, Professional Misconduct, Noncompliance with the Altered Standards of Care
Professional standards should be reviewed by the appropriate state professional licensing boards since there will be variances according to state policies.
Response to Absenteeism
Enforcing accountability raises several ethical questions.
Since verifying reasons for absenteeism would be practically impossible, a “high expectations, no punishment” approach is advisable.
Administrators must realize that not all staff will be available due to illness, childcare issues, and dependent care.
Points to Consider Reflected in the Proposed Workforce Protocol
Transparency
The inclusion of stakeholders in the decision-making process, as well as the presence of communication mechanisms, ensures that those affected will be informed of the developing protocol.
Public Accountability
The inclusion of health care workers in the various levels of the policy-making process, as well as the presence of communication mechanisms, allows policymakers to address the workers promptly regarding any misinterpretations of the protocol.
Responsiveness
Health care professionals’ input in the decision-making process, in addition to the presence of communication mechanisms that allow for the expression of dissatisfaction by the health care professionals, allows for the iterative evaluation and improvement of the protocol.
Proportionality
As personal risk increases, health care workers are able to weigh their own priorities to determine whether they will report to work. They are to decide if the benefits of reporting to work outweigh the burdens of doing so.
Reciprocity
Health care workers, who bear a large portion of the burden of caring for the afflicted, are prioritized for protective equipment and vaccinations in order to minimize their increased risk of infection.
Uniformity of Implementation
Development of workforce management protocol at the State level, the inclusion of health care professionals in the development process, and open communication will help to ensure that members of the health care field statewide will be aware of and approve of the recommended protocol, resulting in policy compliance.
Case Study Responses
Case #1: Custodial staff members are needed to maintain as clean and hygienic an environment as possible to reduce further influenza transmission. Prior to a pandemic, non-clinical employees, including janitorial staff, should be informed of the vital role they will play in a pandemic response. They also should be educated on the nature of a pandemic and how to protect themselves, and they should be encouraged to develop a personal family plan for how to respond to the situation. The hospital should anticipate providing personal protective equipment. Nonetheless, if all recommendations are followed and the employee still is unable or unwilling to report to work, no sanctions or punishment are recommended. The hospital should be prepared to implement a backup strategy.
Case #2: The hospital has an obligation to protect its employees. Given its ability to provide adequate personal protective equipment (PPE) to only half its workforce, the hospital must identify “critically necessary” employees who will be expected to work and who will receive the PPE. All others must not be expected to report to work given the excessive risk they will face. Additionally, the hospital must inform the state, through pre-established modes of communication, of its limited supplies.
Patient Guide
Questions and Answers about Altered Standards of Care:
What is an influenza (flu) pandemic?
A pandemic is a disease outbreak among humans that occurs throughout the world. An influenza pandemic occurs when a new influenza virus begins to cause serious illness and spreads easily from person-to-person. This type of pandemic is likely to be more severe, affect more people, and could cause more deaths than seasonal flu.
What are Altered Standards of Care?
Altered Standards of Care refers to the change in the way health care is delivered during an emergency like an influenza pandemic, the places people will be treated, who will be treating patients, and the resources available for treatment.
During a pandemic, the following are in short supply:
- Medical Care
- Doctors and Nurses
- Hospital Beds (and equipment)
- Medications (including vaccines and antivirals)
In normal times, doctors, nurses and the whole health care system focus on doing the best and the most they can for individual patients. In an emergency, like the influenza pandemic we are experiencing right now, giving every person everything he or she wants and would normally be able to get, may not be possible. Doctors, nurses, and other health care professionals will still attempt to provide patients the best care possible. However, due to the pandemic, there may not be enough medicines, intensive care beds, ventilators (breathing machines), intensive care doctors and nurses, and all the rest of the people and things that make modern hospitals run
All the people who are taking care of the sick at this time are focused on trying to do the ‘greatest good for the greatest number,’ which often involves difficult and painful decisions about which patients get the limited machines and medicines.
Hospitals and communities have prepared for shortages by agreeing to use their limited resources for the people who have the best chance of surviving this awful pandemic. The ‘best chance’ depends on physical characteristics of the patient, how sick he is and how his body responds to the treatment. Other considerations, like what the person does for a living or how much money he makes or who he knows at the hospital, will NOT be part of the decisions about treatment.
The health care providers and community leaders who agreed to this emergency plan did so with great reluctance and only because it seemed to be the least bad option. Working under these new rules causes a lot of distress in nurses, doctors and all health care providers, who are used to providing the best and most they can for everyone.
Will vaccines (“flu shot”) and antiviral medicines work?
The health care experts will decide when a vaccine or antiviral medication can be helpful to either prevent or treat the flu.
How will my family and I get vaccines and antiviral medicine?
Communities have prepared for an influenza pandemic and will publicize where and when treatments are available.
Resources
Altered Standards of Care/Triage
Ontario Health Plan for an Influenza Pandemic – Acute Care Services http://www.health.gov.on.ca/english/providers/program/emu/pan_flu/pan_flu_plan.html
Vaccines and Antivirals
Guidance on Allocating and Targeting Pandemic Influenza Vaccine http://www.pandemicflu.gov/vaccine/allocationguidance.pdf
Vaccines, Vaccine Allocation and Vaccine Research http://www.pandemicflu.gov/vaccine/vacresearch.html#vprioritization
Safety Issues Associated with Pandemic Influenza Vaccines http://www.who.int/vaccine_safety/topics/influenza/pandemic/en/
Pandemic Influenza Vaccines http://www.who.int/immunization/newsroom/vaccine_PI/en/
Workforce Management
Workplace Planning
http://www.pandemicflu.gov/plan/workplaceplanning/index.html
General Planning/ Preparedness
CDC Resources
http://www.cdc.gov/flu/pandemic/preparednesstools.htm
http://www.cdc.gov/flu/pandemic/healthprofessional.htm
Health and Human Services Resources
http://www.hhs.gov/pandemicflu/plan/pdf/HHSPandemicInfluenzaPlan.pdf
http://www.pandemicflu.gov/plan/index.html
http://www.pandemicflu.gov/plan/tab6.html/
http://www.pandemicflu.gov/plan/pdf/medofficesclinics.pdf
http://www.pandemicflu.gov/plan/healthcare/homehealth.html
Pan American Health Organization
http://www.paho.org/Project.asp?SEL=TP&LNG=ENG&ID=534
WHO
http://www.who.int/csr/disease/influenza/PIPGuidance09.pdf
http://www.who.int/ethics/influenza_project/en/
Forum about the Ethics Toolkit
http://panflutoolkit.wordpress.com/
References
Meslin E. M., Alyea J. M., Helft R. P. (2007). Pandemic flu preparedness: ethical issues and recommendations to the Indiana State Department of Health. Indiana University Center for Bioethics. Retrieved from http://www.bioethics.iu.edu/pandemicFluPrep_2007.pdf
Acknowledgement
This project was supported by Grant/Cooperative Agreement Number 5U90TP517024-09 from the Centers for Disease Control and Prevention (CDC). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of CDC.
Indiana Center for Bioethics, www.bioethics.iu.edu
Indiana State Department of Health, www.statehealth.in.gov